LEARN ABOUT CARDIAC ISSUES
CLINICAL EXPERTISE
Coronary Artery Disease
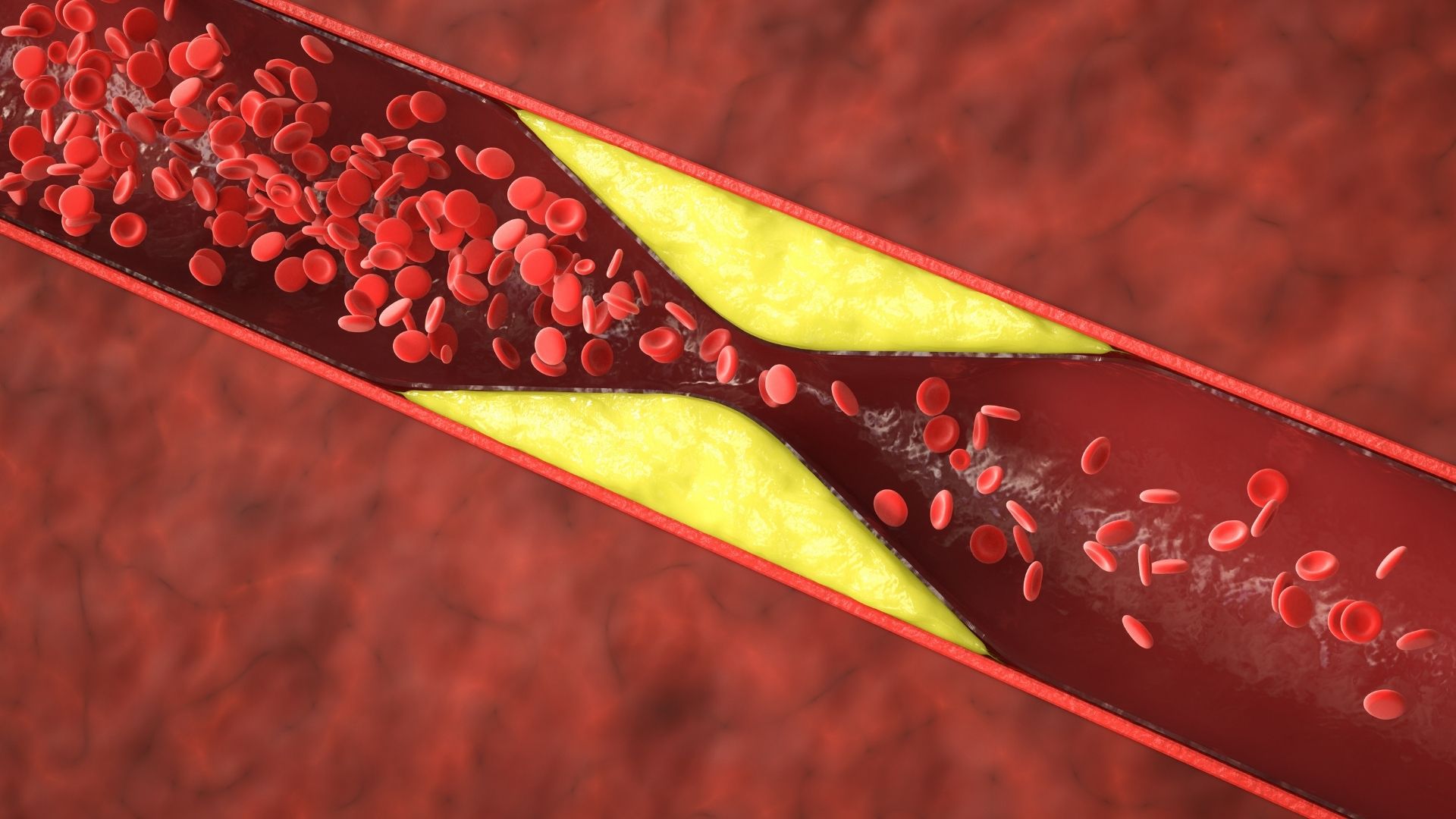
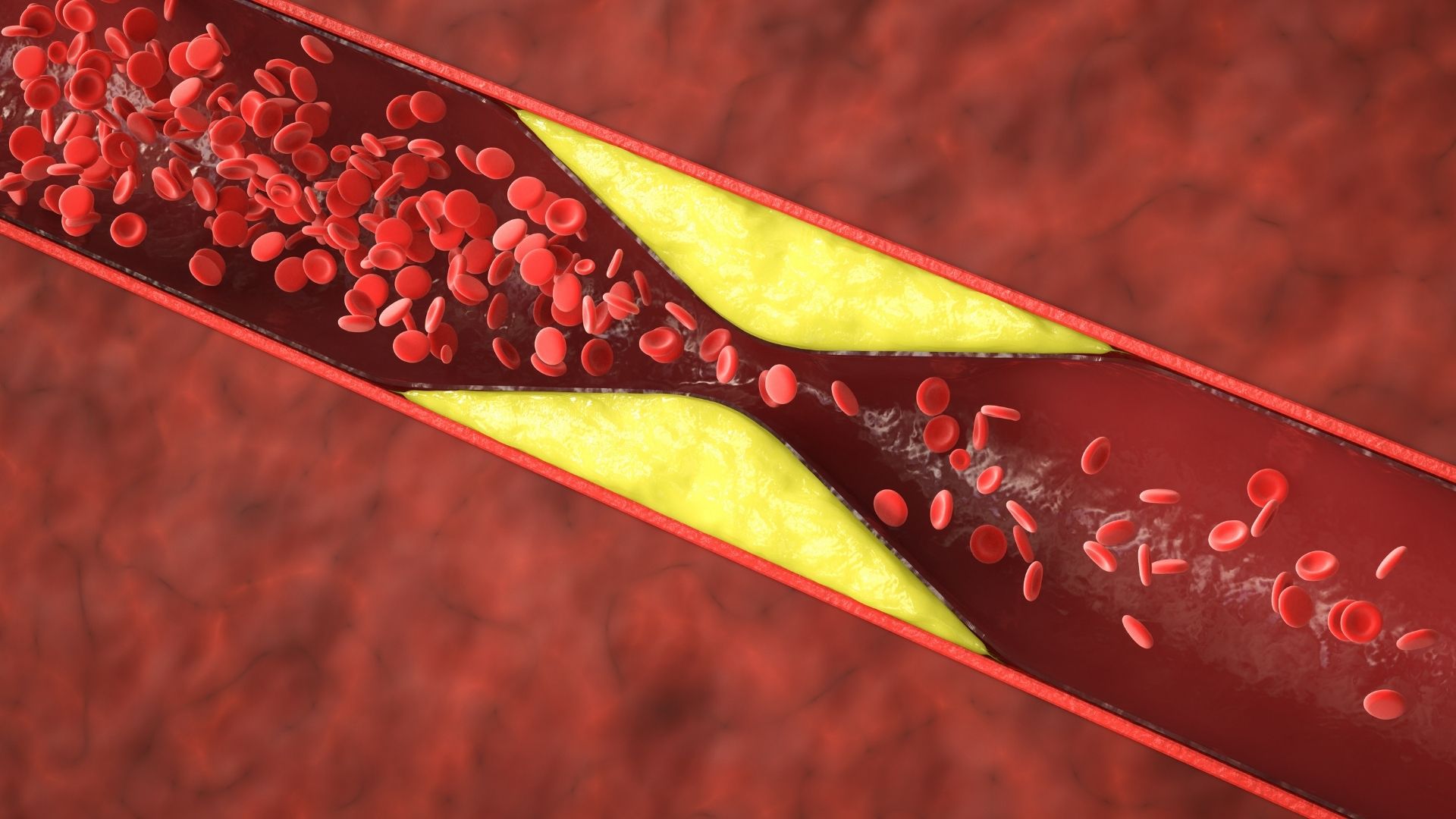
Coronary artery disease (CAD) is a common heart condition where the arteries that supply blood to your heart become narrowed or blocked by fatty deposits called plaques. This buildup, known as atherosclerosis, reduces blood flow to the heart and can cause chest pain (angina), shortness of breath, or even a heart attack.
CAD develops over many years and is often linked to lifestyle and health factors. Common causes and risk factors include high blood pressure, high cholesterol, smoking, diabetes, obesity, physical inactivity, and a family history of heart disease. Stress and an unhealthy diet can also contribute.
The good news is that CAD can often be managed or even prevented with lifestyle changes. Stopping smoking, eating a heart-healthy diet (low in saturated fats and high in fruits and vegetables), exercising regularly, and maintaining a healthy weight are key steps. Doctors may also prescribe medications to control blood pressure, cholesterol, or prevent blood clots. In more serious cases, procedures like angioplasty or bypass surgery may be needed to restore blood flow.
Understanding your risk and making healthy choices early on can significantly reduce your chances of developing serious heart problems related to coronary artery disease.
Hypertension
Hypertension, or high blood pressure, is a common condition where the force of blood against your artery walls is consistently too high. Over time, this can strain your heart and blood vessels, increasing the risk of heart disease, stroke, kidney problems, and other serious health issues.
Blood pressure is measured with two numbers: systolic (the top number) and diastolic (the bottom number). A normal reading is usually around 120/80 mmHg. Hypertension is typically diagnosed when readings are 140/90 mmHg or higher on repeated checks. For some, especially those with other health risks, even slightly lower readings may be considered high.
There’s often no obvious cause, which is why it’s sometimes called the “silent killer.” However, contributing factors include being overweight, having a sedentary lifestyle, high salt intake, excessive alcohol, stress, smoking, and a family history of hypertension.
Treatment starts with lifestyle changes—such as reducing salt, eating a balanced diet, exercising regularly, limiting alcohol, quitting smoking, and managing stress. If lifestyle changes aren’t enough, doctors may prescribe medications to lower blood pressure.
Regular monitoring and early treatment are key to avoiding long-term complications. Many people live healthy lives by keeping their blood pressure under control.
Palpitations and Syncope
Palpitations are sensations of a rapid, fluttering, or pounding heartbeat. They can be caused by stress, caffeine, dehydration, or underlying heart conditions like arrhythmias. While often harmless, persistent palpitations may indicate a more serious issue.
Syncope, or fainting, occurs when there is a temporary drop in blood flow to the brain, leading to a brief loss of consciousness. Causes range from dehydration and low blood pressure to heart rhythm disorders and neurological conditions. Some people experience syncope due to vasovagal reflexes triggered by pain, fear, or standing too long.
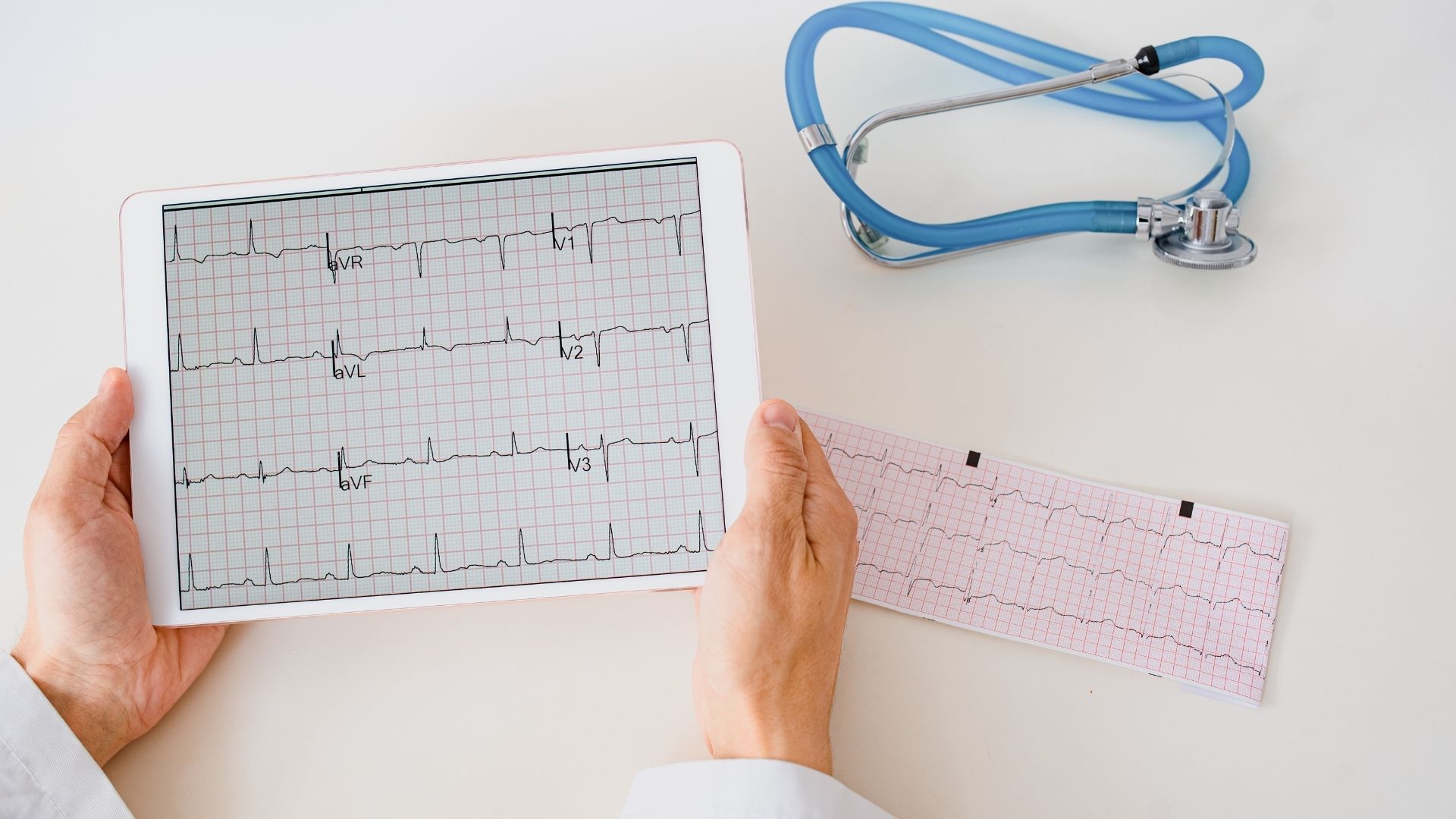
Diagnosis typically involves electrocardiograms (ECG), Holter monitoring, echocardiograms, and tilt table tests to assess heart function and blood pressure regulation. Blood tests may also help identify underlying conditions.
Treatment depends on the cause. Lifestyle changes, like staying hydrated, reducing caffeine, and managing stress can help with palpitations. Medications may be prescribed for arrhythmias or blood pressure issues. In some cases, pacemakers or implantable monitors are used to track and regulate heart rhythms. If syncope is linked to heart disease, addressing the underlying condition is crucial.
Regular check-ups and early intervention can help manage symptoms and prevent complications. If fainting occurs frequently, seeking medical advice is essential.

HEART FAILURE
Heart failure is a condition where the heart doesn’t pump blood as well as it should. It doesn’t mean the heart has stopped working, but rather that it’s struggling to meet the body’s needs. It can develop slowly over time or come on suddenly.
Common causes include coronary artery disease, high blood pressure, previous heart attacks, heart valve problems, or certain heart rhythm disorders. Long-term alcohol use, diabetes, and untreated lung disease can also contribute.
Signs and symptoms to watch for include:
• Shortness of breath, especially when lying flat or during exertion
• Fatigue or weakness
• Swollen legs, ankles, or belly
• Sudden weight gain from fluid retention
• Persistent coughing or wheezing
• Difficulty exercising or reduced ability to do everyday activities
If you notice these signs, it’s important to see a cardiologist promptly. Early diagnosis and treatment can prevent the condition from worsening.
Treatment usually includes lifestyle changes (like reducing salt, controlling weight, quitting smoking), medications to ease symptoms and support heart function, and sometimes devices. These may include pacemakers, implantable defibrillators (ICDs) to prevent sudden cardiac death, or cardiac resynchronization therapy (CRT) to help both sides of the heart beat in sync.
With proper care, many people with heart failure live full, active lives.

Cardiac Arrhythmias
Arrhythmias are irregular heart rhythms—when the heart beats too fast, too slow, or unevenly. They happen when the electrical signals that control your heartbeat are disrupted. Some arrhythmias are harmless and may cause no symptoms, while others can lead to dizziness, palpitations, fatigue, or even fainting.
Not all arrhythmias need medical treatment. Many are mild and only require lifestyle changes, such as reducing caffeine and alcohol, managing stress, quitting smoking, or correcting sleep disorders like sleep apnea. However, some arrhythmias can increase the risk of stroke or heart failure and need medical care.
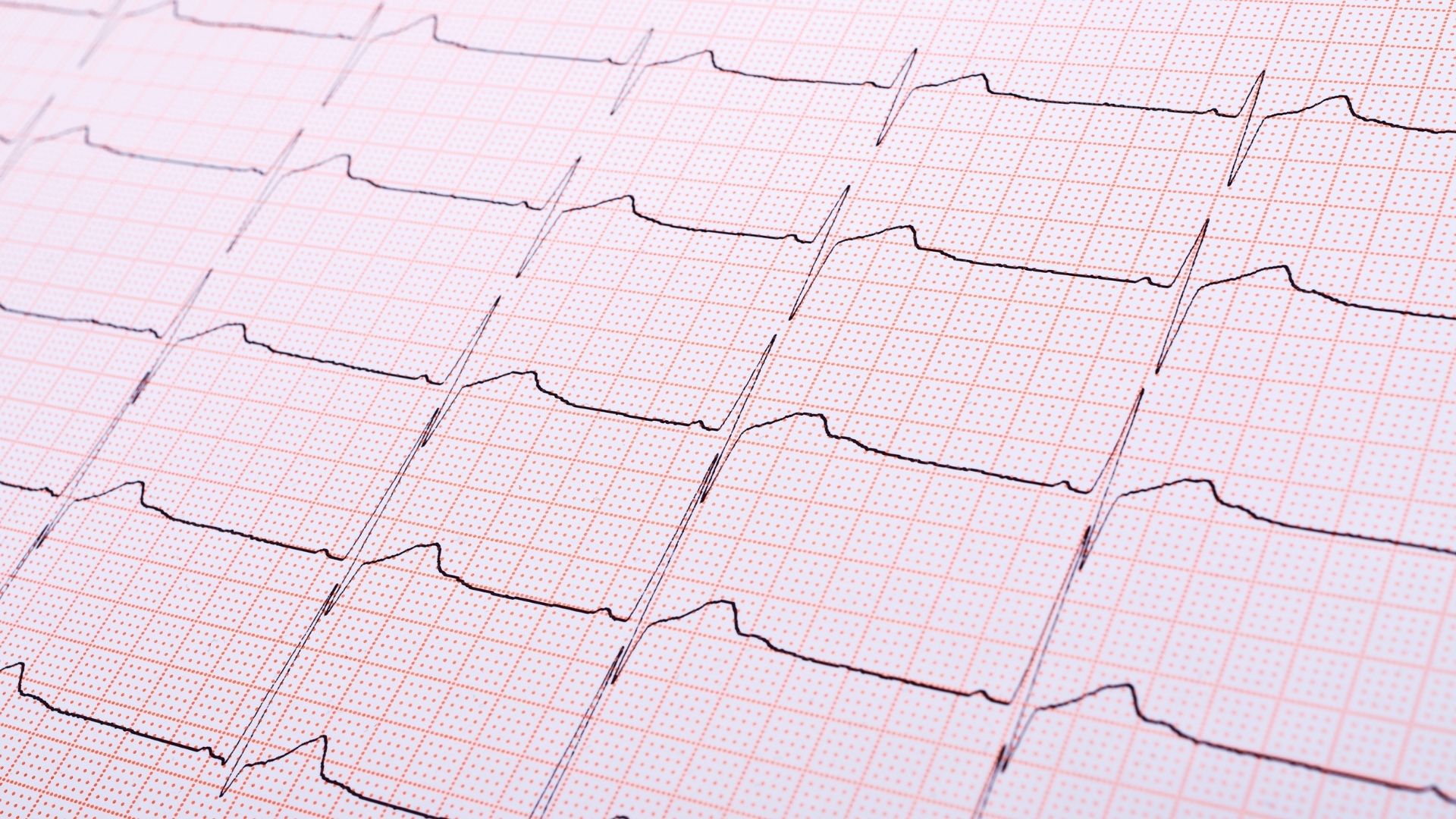
Diagnosing an arrhythmia often involves an electrocardiogram (ECG), which records the heart’s electrical activity. If the irregular rhythm is occasional, your doctor may recommend a Holter monitor or other wearable device to track your heart over time.
Treatment depends on the type and severity. It may include medications to control heart rate or rhythm, or to prevent blood clots. In some cases, procedures like catheter ablation (which targets abnormal heart tissue) or implanted devices like pacemakers or defibrillators are used to regulate the heartbeat.
If you’re experiencing unusual heartbeats, it’s worth getting checked—many arrhythmias are manageable once properly identified.
Valve Diseases
Heart valve disease occurs when one or more of the valves in your heart don’t open or close properly, affecting blood flow. The most commonly affected valves are the mitral and aortic valves.
Mitral valve disease can include stenosis (narrowing) or regurgitation (leakage). A leaky mitral valve can cause fatigue, breathlessness, and irregular heartbeats. Aortic valve disease, especially aortic stenosis, is common with age and can lead to chest pain, breathlessness, dizziness, or even fainting, especially during exertion.
Diagnosis usually begins with a stethoscope exam, followed by an echocardiogram (heart ultrasound), which shows how well the valves are working. Additional tests like ECG, CT scans, or cardiac MRI may be used for detailed assessment.
Many valve problems progress slowly, so regular check-ups and scans are crucial, even if you feel fine. Monitoring helps decide the right time for treatment—before irreversible heart damage occurs.
Cardiac Screening
Cardiac screening before starting or continuing sporting activities is important—especially for middle-aged individuals—because the heart may have silent conditions that only become apparent during intense exercise. While physical activity is generally good for heart health, underlying problems like coronary artery disease, arrhythmias, or valve issues can pose serious risks when the heart is under stress.
In some people, the first sign of a heart issue may be chest pain, palpitations, dizziness, or even a sudden cardiac event during exercise. This is why pre-participation screening is recommended, especially if you’re over 40 or have risk factors such as high blood pressure, high cholesterol, diabetes, a family history of heart disease, or if you’ve been inactive for a long time.
Cardiac screening often includes a medical history review, physical examination, and an ECG (electrocardiogram). Depending on the findings, additional tests like an echocardiogram or a stress test may be advised.
The goal is not to stop you from exercising, but to ensure it’s safe and tailored to your heart’s condition. Early detection of issues allows for timely treatment or adjustments in activity level, helping prevent complications while supporting a healthy, active lifestyle
Dyslipidaemia
Dyslipidaemia means having abnormal levels of fats (lipids) in the blood—usually too much “bad” cholesterol (LDL), too little “good” cholesterol (HDL), or high levels of triglycerides. Over time, this can lead to plaque buildup in the arteries, increasing the risk of heart attack, stroke, and other cardiovascular problems.
A common cause is unhealthy dietary habits, such as eating foods high in saturated fats, trans fats, and processed sugars. A lack of physical activity, being overweight, smoking, and excessive alcohol use also play a role.
Some people have a genetic condition called familial hypercholesterolaemia, where high cholesterol runs in the family and starts early in life—even with a healthy lifestyle. These individuals are at much higher risk and usually require medical treatment.
Dyslipidaemia is often silent, without symptoms, so it’s important to check cholesterol levels regularly—especially after age 40 or if you have risk factors like high blood pressure or diabetes.
Treatment includes lifestyle changes: a heart-healthy diet (rich in fruits, vegetables, whole grains, and healthy fats), regular exercise, weight loss, and quitting smoking. If cholesterol levels remain high, doctors may prescribe statins or other medications to lower LDL and protect the heart. Managing dyslipidaemia greatly reduces cardiovascular risk.
LEARN ABOUT CARDIAC ISSUES
CLINICAL EXPERTISE
Coronary Artery Disease
Coronary artery disease (CAD) is a common heart condition where the arteries that supply blood to your heart become narrowed or blocked by fatty deposits called plaques. This buildup, known as atherosclerosis, reduces blood flow to the heart and can cause chest pain (angina), shortness of breath, or even a heart attack.
CAD develops over many years and is often linked to lifestyle and health factors. Common causes and risk factors include high blood pressure, high cholesterol, smoking, diabetes, obesity, physical inactivity, and a family history of heart disease. Stress and an unhealthy diet can also contribute.
The good news is that CAD can often be managed or even prevented with lifestyle changes. Stopping smoking, eating a heart-healthy diet (low in saturated fats and high in fruits and vegetables), exercising regularly, and maintaining a healthy weight are key steps. Doctors may also prescribe medications to control blood pressure, cholesterol, or prevent blood clots. In more serious cases, procedures like angioplasty or bypass surgery may be needed to restore blood flow.
Understanding your risk and making healthy choices early on can significantly reduce your chances of developing serious heart problems related to coronary artery disease.
Hypertension
Hypertension, or high blood pressure, is a common condition where the force of blood against your artery walls is consistently too high. Over time, this can strain your heart and blood vessels, increasing the risk of heart disease, stroke, kidney problems, and other serious health issues.
Blood pressure is measured with two numbers: systolic (the top number) and diastolic (the bottom number). A normal reading is usually around 120/80 mmHg. Hypertension is typically diagnosed when readings are 140/90 mmHg or higher on repeated checks. For some, especially those with other health risks, even slightly lower readings may be considered high.
There’s often no obvious cause, which is why it’s sometimes called the “silent killer.” However, contributing factors include being overweight, having a sedentary lifestyle, high salt intake, excessive alcohol, stress, smoking, and a family history of hypertension.
Treatment starts with lifestyle changes—such as reducing salt, eating a balanced diet, exercising regularly, limiting alcohol, quitting smoking, and managing stress. If lifestyle changes aren’t enough, doctors may prescribe medications to lower blood pressure.
Regular monitoring and early treatment are key to avoiding long-term complications. Many people live healthy lives by keeping their blood pressure under control.

Palpitations and Syncope
Palpitations are sensations of a rapid, fluttering, or pounding heartbeat. They can be caused by stress, caffeine, dehydration, or underlying heart conditions like arrhythmias. While often harmless, persistent palpitations may indicate a more serious issue.
Syncope, or fainting, occurs when there is a temporary drop in blood flow to the brain, leading to a brief loss of consciousness. Causes range from dehydration and low blood pressure to heart rhythm disorders and neurological conditions. Some people experience syncope due to vasovagal reflexes triggered by pain, fear, or standing too long.
Diagnosis typically involves electrocardiograms (ECG), Holter monitoring, echocardiograms, and tilt table tests to assess heart function and blood pressure regulation. Blood tests may also help identify underlying conditions.
Treatment depends on the cause. Lifestyle changes, like staying hydrated, reducing caffeine, and managing stress can help with palpitations. Medications may be prescribed for arrhythmias or blood pressure issues. In some cases, pacemakers or implantable monitors are used to track and regulate heart rhythms. If syncope is linked to heart disease, addressing the underlying condition is crucial.
Regular check-ups and early intervention can help manage symptoms and prevent complications. If fainting occurs frequently, seeking medical advice is essential.

HEART FAILURE
Heart failure is a condition where the heart doesn’t pump blood as well as it should. It doesn’t mean the heart has stopped working, but rather that it’s struggling to meet the body’s needs. It can develop slowly over time or come on suddenly.
Common causes include coronary artery disease, high blood pressure, previous heart attacks, heart valve problems, or certain heart rhythm disorders. Long-term alcohol use, diabetes, and untreated lung disease can also contribute.
Signs and symptoms to watch for include:
• Shortness of breath, especially when lying flat or during exertion
• Fatigue or weakness
• Swollen legs, ankles, or belly
• Sudden weight gain from fluid retention
• Persistent coughing or wheezing
• Difficulty exercising or reduced ability to do everyday activities
If you notice these signs, it’s important to see a cardiologist promptly. Early diagnosis and treatment can prevent the condition from worsening.
Treatment usually includes lifestyle changes (like reducing salt, controlling weight, quitting smoking), medications to ease symptoms and support heart function, and sometimes devices. These may include pacemakers, implantable defibrillators (ICDs) to prevent sudden cardiac death, or cardiac resynchronization therapy (CRT) to help both sides of the heart beat in sync.
With proper care, many people with heart failure live full, active lives.
Cardiac Arrhythmias
Arrhythmias are irregular heart rhythms—when the heart beats too fast, too slow, or unevenly. They happen when the electrical signals that control your heartbeat are disrupted. Some arrhythmias are harmless and may cause no symptoms, while others can lead to dizziness, palpitations, fatigue, or even fainting.
Not all arrhythmias need medical treatment. Many are mild and only require lifestyle changes, such as reducing caffeine and alcohol, managing stress, quitting smoking, or correcting sleep disorders like sleep apnea. However, some arrhythmias can increase the risk of stroke or heart failure and need medical care.
Diagnosing an arrhythmia often involves an electrocardiogram (ECG), which records the heart’s electrical activity. If the irregular rhythm is occasional, your doctor may recommend a Holter monitor or other wearable device to track your heart over time.
Treatment depends on the type and severity. It may include medications to control heart rate or rhythm, or to prevent blood clots. In some cases, procedures like catheter ablation (which targets abnormal heart tissue) or implanted devices like pacemakers or defibrillators are used to regulate the heartbeat.
If you’re experiencing unusual heartbeats, it’s worth getting checked—many arrhythmias are manageable once properly identified.
Valve Diseases
Heart valve disease occurs when one or more of the valves in your heart don’t open or close properly, affecting blood flow. The most commonly affected valves are the mitral and aortic valves.
Mitral valve disease can include stenosis (narrowing) or regurgitation (leakage). A leaky mitral valve can cause fatigue, breathlessness, and irregular heartbeats. Aortic valve disease, especially aortic stenosis, is common with age and can lead to chest pain, breathlessness, dizziness, or even fainting, especially during exertion.
Diagnosis usually begins with a stethoscope exam, followed by an echocardiogram (heart ultrasound), which shows how well the valves are working. Additional tests like ECG, CT scans, or cardiac MRI may be used for detailed assessment.
Many valve problems progress slowly, so regular check-ups and scans are crucial, even if you feel fine. Monitoring helps decide the right time for treatment—before irreversible heart damage occurs.
Cardiac Screening
Cardiac screening before starting or continuing sporting activities is important—especially for middle-aged individuals—because the heart may have silent conditions that only become apparent during intense exercise. While physical activity is generally good for heart health, underlying problems like coronary artery disease, arrhythmias, or valve issues can pose serious risks when the heart is under stress.
In some people, the first sign of a heart issue may be chest pain, palpitations, dizziness, or even a sudden cardiac event during exercise. This is why pre-participation screening is recommended, especially if you’re over 40 or have risk factors such as high blood pressure, high cholesterol, diabetes, a family history of heart disease, or if you’ve been inactive for a long time.
Cardiac screening often includes a medical history review, physical examination, and an ECG (electrocardiogram). Depending on the findings, additional tests like an echocardiogram or a stress test may be advised.
The goal is not to stop you from exercising, but to ensure it’s safe and tailored to your heart’s condition. Early detection of issues allows for timely treatment or adjustments in activity level, helping prevent complications while supporting a healthy, active lifestyle
Dyslipidaemia
c means having abnormal levels of fats (lipids) in the blood—usually too much “bad” cholesterol (LDL), too little “good” cholesterol (HDL), or high levels of triglycerides. Over time, this can lead to plaque buildup in the arteries, increasing the risk of heart attack, stroke, and other cardiovascular problems.
A common cause is unhealthy dietary habits, such as eating foods high in saturated fats, trans fats, and processed sugars. A lack of physical activity, being overweight, smoking, and excessive alcohol use also play a role.
Some people have a genetic condition called familial hypercholesterolaemia, where high cholesterol runs in the family and starts early in life—even with a healthy lifestyle. These individuals are at much higher risk and usually require medical treatment.
Dyslipidaemia is often silent, without symptoms, so it’s important to check cholesterol levels regularly—especially after age 40 or if you have risk factors like high blood pressure or diabetes.
Treatment includes lifestyle changes: a heart-healthy diet (rich in fruits, vegetables, whole grains, and healthy fats), regular exercise, weight loss, and quitting smoking. If cholesterol levels remain high, doctors may prescribe statins or other medications to lower LDL and protect the heart. Managing dyslipidaemia greatly reduces cardiovascular risk.
